Designing More Useful Bacteria
- BiotechnologyInternational News
- No Comment
- 490
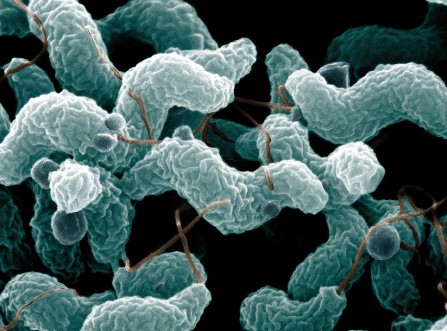
In a step forward for genetic engineering and synthetic biology, researchers have modified a strain of Escherichia coli bacteria to be immune to natural viral infections while also minimizing the potential for the bacteria or their modified genes to escape into the wild.
Results are published March 15 in Nature.
“We believe we have developed the first technology to design an organism that can’t be infected by any known virus,” said the study’s first author, Akos Nyerges, research fellow in genetics in the lab of George Church in the Blavatnik Institute at Harvard Medical School and the Wyss Institute for Biologically Inspired Engineering.
“We can’t say it’s fully virus-resistant, but so far, based on extensive laboratory experiments and computational analysis, we haven’t found a virus that can break it,” Nyerges said.
The work also provides the first built-in safety measure that prevents modified genetic material from being incorporated into natural cells, he said.
The authors said their work suggests a general method for making any organism immune to viruses and preventing gene flow into and out of genetically modified organisms (GMOs). Such biocontainment strategies are of increasing interest as groups explore the safe deployment of GMOs for growing crops, reducing disease spread, generating biofuels, and removing pollutants from open environments.
Building on what came before
The findings build on earlier efforts by genetic engineers to achieve a helpful, safe, virus-resistant bacterium.
In 2022, a group from the University of Cambridge thought they’d made an E. coli strain immune to viruses. But then Nyerges teamed up with research fellow Siân Owen and graduate student Eleanor Rand in the lab of co-author Michael Baym, assistant professor of biomedical informatics in the Blavatnik Institute at HMS. When they sampled local sites rife with E. coli, including chicken sheds, rat nests, sewage, and the Muddy River down the street from the HMS campus, they discovered viruses that could still infect the modified bacteria.
Discovering that the bacteria weren’t fully virus-resistant “was a bummer,” Nyerges said.
The initial method had involved genetically reprogramming E. coli to make all their life-sustaining proteins from 61 sets of genetic building blocks, or codons, instead of the naturally occurring 64. The idea was that viruses wouldn’t be able to hijack the cells because they couldn’t replicate without the missing codons.
The HMS team, however, figured out that deleting codons wasn’t enough. Some viruses were bringing in their own equipment to get around the missing pieces.
So, Nyerges and colleagues developed a way to change what those codons tell an organism to make — something scientists hadn’t done to this extent in living cells.
By Harvard Medical School
https://www.sciencedaily.com/releases/2023/03/230315132359.htm