Failed Clinical Trial Leads to Scientific Breakthrough: Investigating Cancer Drug Toxicity Leads to Critical Discovery
- Biotechnology
- No Comment
- 211
Researchers uncover a new strategy to avoid cancer immunotherapy side effects.
It’s not often that a failed clinical trial leads to a scientific breakthrough.
When patients in the UK started experiencing negative side effects during a cancer immunotherapy trial, researchers at La Jolla Institute for Immunology (LJI) Center for Cancer Immunotherapy and University of Liverpool went back, examined the data, and worked with patient samples to determine what went wrong.
“This work shows the importance of learning from early stage clinical trials,” says La Jolla Institute for Immunology (LJI) Professor Pandurangan Vijayanand, M.D., Ph.D., who co-led the new research with Christian H. Ottensmeier, M.D., Ph.D., FRCP, a professor with the University of Liverpool, The Clatterbridge Cancer Centre NHS Foundation Trust, and adjunct professor at LJI.
Limited success with immunotherapies
Both Vijayanand and Ottensmeier are physician-scientists, and Ottensmeier is an attending oncologist who treats solid tumor patients. In just the last decade, he has seen more and more patients thrive thanks to advances in immunotherapies, which work with the immune system to kill cancers.
“In the oncology world, immunotherapy has revolutionized the way we think about treatment,” says Ottensmeier. “We can give immunotherapies to patients even with metastatic and spreading disease, and then just three years later wave goodbye and tell them their cancer is cured. This is an astounding change.”
Unfortunately, only around 20 to 30 percent of solid cancer patients given immunotherapies go into long-term remission. Some people see no change after immunotherapy, but others develop serious problems in their lungs, bowel, and even skin during treatment. These side effects can be debilitating, even fatal, and these patients are forced to stop receiving the immunotherapy.
Important lessons from a clinical trial
The researchers at LJI and the University of Liverpool worked with samples from a recent clinical trial in the UK for patients with head and neck cancers. The patients were given an oral cancer immunotherapy called a PI3Kd inhibitor. At the time, PI3Kd inhibitors had proven effective for B cell lymphomas but had not yet been tested in solid tumors.
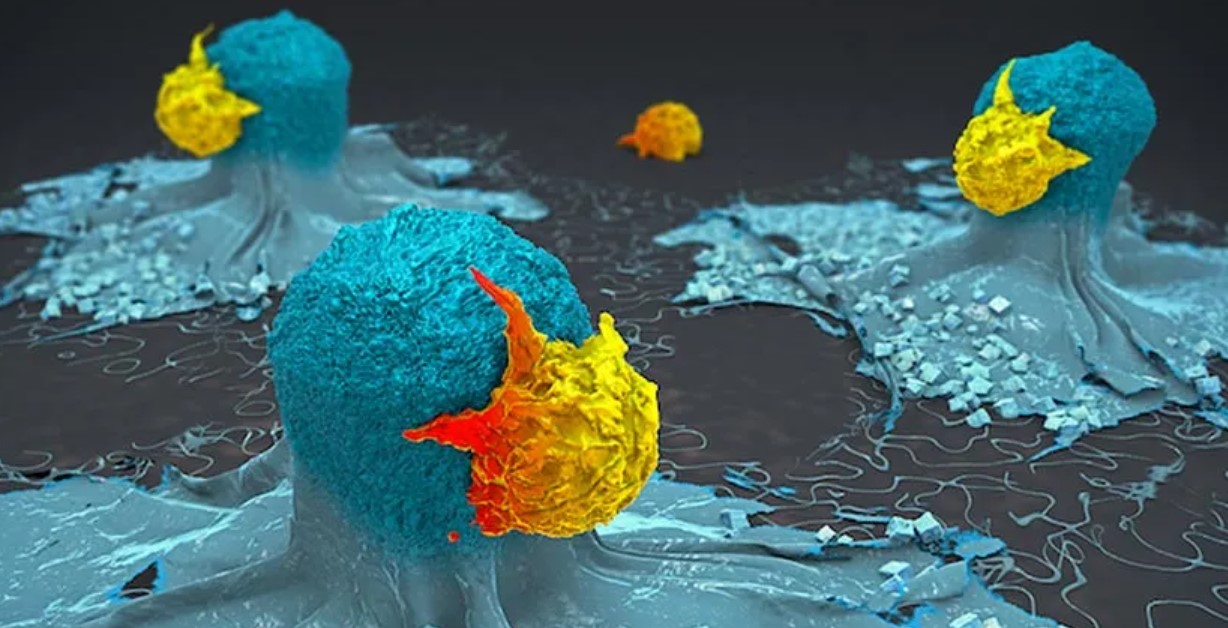
PI3Kd inhibitors are new to the cancer immunotherapy scene, but they hold promise for their ability to inhibit “regulatory” T cells (Tregs). Tregs normally try to stop other T cells, called effector T cells, from targeting the body’s own tissues. Oncologists inhibit Tregs inside tumors so effector T cells can let loose and generate cancer-killing CD8+ T cells.
“Having an oral tablet that can take off the brakes—the Tregs—can be a great asset for oncologists,” says Vijayanand.
Unfortunately, 12 of the 21 patients in the trial had to discontinue treatment early because they developed inflammation in the colon, a condition called colitis. “We thought this drug wouldn’t be toxic, so why was this happening?” says Vijayanand.
LJI Instructor Simon Eschweiler, Ph.D., spearheaded the effort to go back and see exactly how PI3Kd inhibitor treatment affected immune cells in these patients. Using single-cell genomic sequencing, he showed that in the process of increasing tumor-fighting T cells in tumors, the PI3Kd inhibitor, also blocked a specific Treg cell subset from protecting the colon. Without Tregs on the job, pathogenic T cells, called Th17 and Tc17 cells, moved in and caused inflammation and colitis.
By
https://scitechdaily.com/failed-clinical-trial-leads-to-scientific-breakthrough-investigating-cancer-drug-toxicity-leads-to-critical-discovery/