Scientists Discover Key to Stopping Aggressive Prostate Cancer Subtype
- Biotechnology
- No Comment
- 191
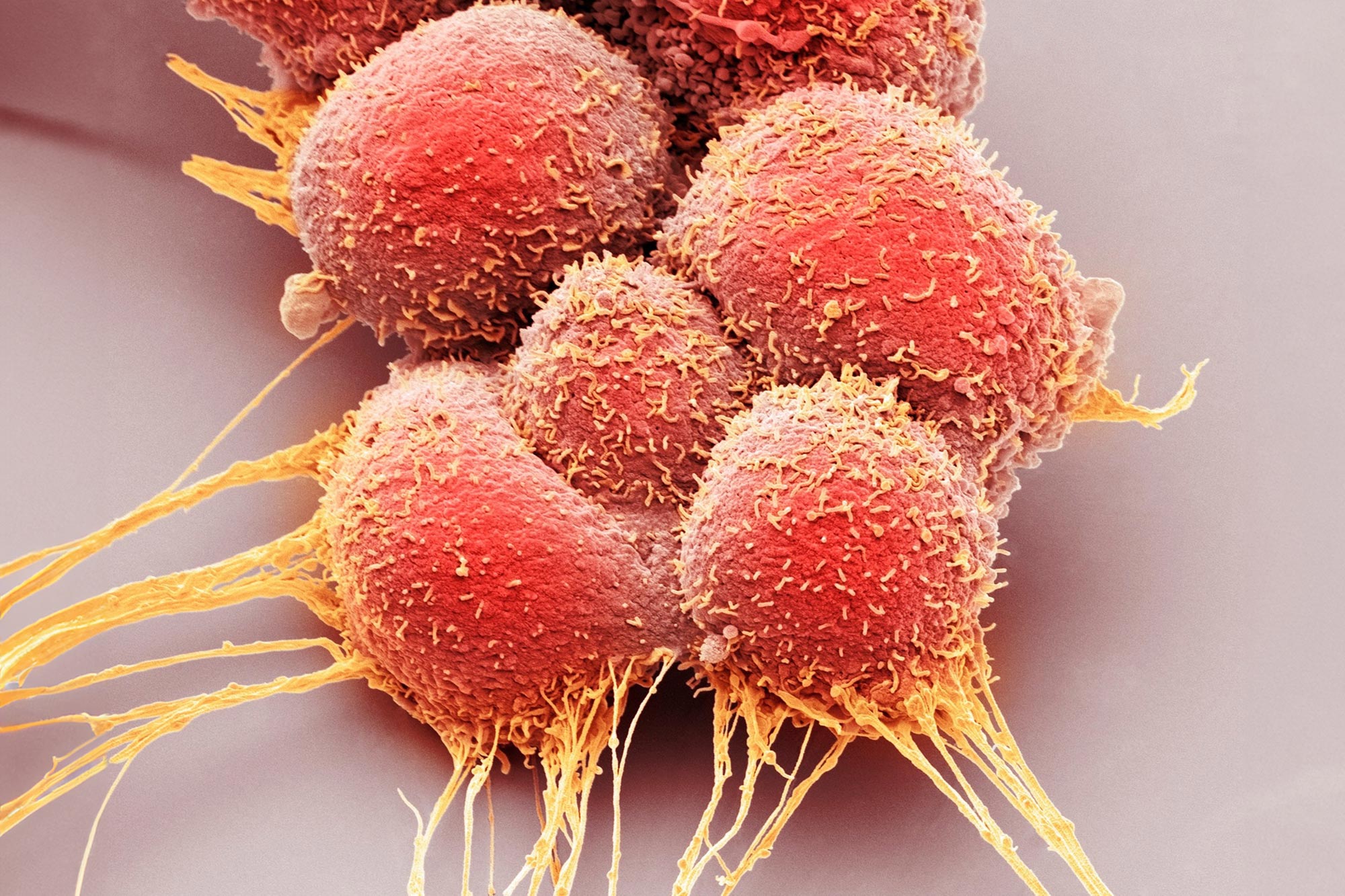
University of Michigan researchers have made significant strides in understanding and treating a new, aggressive subtype of prostate cancer linked to the CDK12 gene.
They’ve developed a mouse model to study the gene’s impact, discovered how its loss induces DNA damage, and created an innovative oral therapy that targets CDK12 and CDK13, showing promise in preliminary tests. This therapy, when combined with existing treatments, could potentially overcome the common problem of resistance in cancer treatment.
Breakthrough in Prostate Cancer Research
After scientists at the University of Michigan Rogel Cancer Center first discovered a new subtype of aggressive prostate cancer, they knew they needed to understand how this genetic alteration was driving cancer and how to target it with treatment.
In two new papers, each published in the journal Cell Reports Medicine, they do both, describing the mechanisms of how alterations in the CDK12 gene drive prostate cancer development and reporting on a promising degrader that targets CDK12 and a related gene to destroy tumors.
Role of CDK12 in Aggressive Cancer Forms
Investigators previously found loss of the CDK12 gene in about 7% of patients with metastatic prostate cancer, suggesting this alteration may be linked to a more aggressive form of the disease. This was discovered from DNA and RNA sequencing from patient tumor samples. CDK12 also plays a role in some ovarian cancers.
To understand how CDK12 loss impacts cells on a molecular level, researchers created a mouse model to try to parallel the genetic alterations they were seeing in human prostate cancers.
“What was quite surprising was when we created CDK12 loss in a mouse prostate, this caused precursor lesions to form in the mouse prostate. Then, when we added loss of the p53 oncogene, the mice developed bona fide invasive prostate cancer,” said senior author Arul M. Chinnaiyan, M.D., Ph.D., director of the Michigan Center for Translational Pathology and S.P. Hicks Professor of Pathology at Michigan Medicine. “It will be an addition to the field to have a genetically engineered mouse model that parallels what we see in human prostate cancer.”
Linking Gene Loss and DNA Damage
With the mouse model, researchers then discovered the of mechanism of how CDK12 loss induces DNA damage. The loss of this gene activates other known cancer driver genes, causing them to be overexpressed at a high level while also causing DNA to be replicated very rapidly. The collision of these two processes leads to DNA damage.
“These back-to-back studies taken together are quite impressive. We created an animal model and then deciphered the mechanisms of how CDK12 loss actually drives prostate cancer,” Chinnaiyan said.
Therapeutic Advances and Gene Targeting
The team also found that a partner gene, CDK13, is important in targeting the alteration therapeutically. They developed a potential therapy designed to degrade CDK12 and CDK13. Testing in cell lines and mice showed the degrader specifically binds to CDK12 and CDK13 and stops the growth of cancer cells over normal cells. The degrader can be absorbed orally and would not need to be delivered intravenously. This is notable as most protein degraders are too large to be absorbed orally, which has limited their potential in drug development.
Combining Therapies to Overcome Resistance
Further, they found that knocking down CDK12/13 activated the AKT pathway, which plays a role in cancer development. Combining the CDK12/13 degrader with existing therapies targeting AKT resulted in a synergistic effect in destroying cancer cells. This suggests the potential to combine a CDK12/13 degrader with other approved therapies.
“It’s well known that single therapies for cancer treatment have been challenging. Oftentimes patients develop resistance. If we can find the right combination, we could prevent resistance mechanisms from occurring. That’s one of the benefits of finding an FDA-approved agent to combine with CDK12/13 degraders,” Chinnaiyan said. “This study also highlights an international collaboration with Ke Ding, Ph.D., a medicinal chemist at the Shanghai Institute of Chemistry, in the development of orally bioavailable CDK12/13 degraders.”
Next Steps Toward Clinical Trials
Researchers plan to further develop the CDK12/13 degrader with a goal of moving it to a clinical trial.